Implementation roadmap
- Home
- Programs
- Shared care for allergy
- Implementation roadmap
Delivering better allergy care across Australia - a coordinated national plan
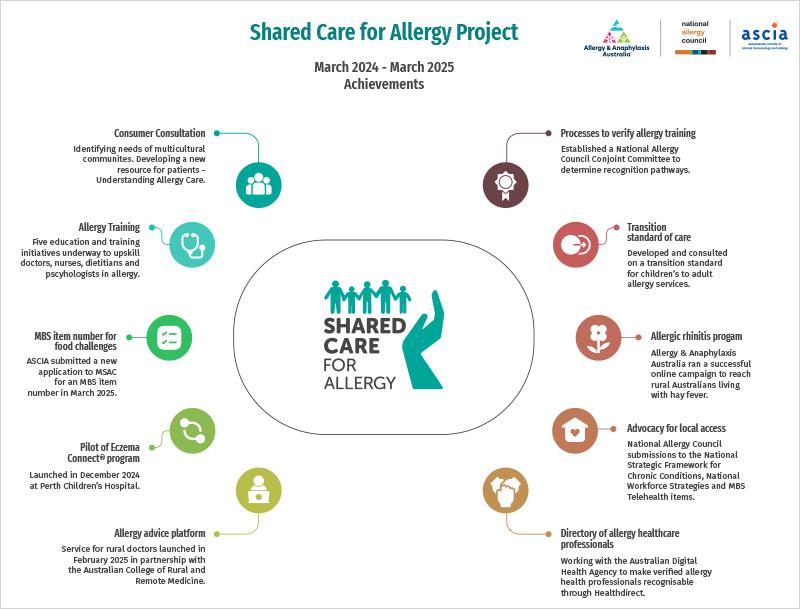
The Shared Care for Allergy Project is making real improvements to allergy care across Australia, focusing on areas that need it most - rural, regional and remote communities. The National Allergy Council, in partnership with the Australasian Society of Clinical Immunology and Allergy (ASCIA) and Allergy & Anaphylaxis Australia, is delivering a clear and practical Implementation Roadmap that outlines the national steps being taken to improve care. The roadmaps are informed by national consultations with people with allergies and those who care for them, healthcare professionals and expert working groups. Each roadmap sets out a clear plan to improve the allergy care system with exciting new pilots, training for health professionals, and new digital tools to support care.
Implementation Roadmap 2025-2026
View the roadmap to learn more about the activities progressed between April 2025 and May 2026.

What difference are we making?

MBS item number for food challenges
The Australasian Society of Clinical Immunology and Allergy (ASCIA) has applied to the Government for a Medicare Benefits Schedule (MBS) item number for medically supervised oral food challenges (OFC). There are long waiting times for OFC in the public system. With an MBS item number, more people should be able to access OFC in private allergy specialist clinics.

ASCIA e-training promotion
ASCIA provides free online training in anaphylaxis for healthcare professionals, which is accessible, consistent and evidence-based. To increase the number of course completions, ASCIA is working with peak health professional bodies to approve the courses for continuing professional development (CPD) activities, for GPs, nurses, dietitians and pharmacists. ASCIA will continue to promote courses through medical conferences, social media and newsletters.

New allergy training pathways and networks
Continue to develop and deliver education and training pilots for doctors, nurses, dietitians and psychologists that will increase the number of healthcare professionals providing quality allergy care to patients in rural and regional areas. Set up a Regional and Rural Clinical Allergy Network to make sure newly trained doctors stay connected and are able to access ongoing support and mentorship from experienced doctors, including clinical immunology/allergy specialists and each other.

Allergy education and support for diverse groups
Education and support for people with allergic conditions and their carers in regional, rural and remote areas and from different cultural and language backgrounds. Allergy & Anaphylaxis Australia will promote the newly developed Understanding Allergy Care web pages on the Allergy & Anaphylaxis website and their National Allergy Helpline. To support multicultural communities, Allergy & Anaphylaxis Australia will develop and pilot an allergy awareness presentation to be delivered by multicultural health workers.

Increase awareness of patient and carer support organisations
Allergy & Anaphylaxis Australia (A&AA) is a patient support organisation dedicated to helping people with allergy and their carers in understanding and managing their allergic condition(s). The ASCIA website information is being updated to include links at the start of each document to make sure healthcare professionals and their patients are aware of the free National Allergy Helpline and the services offered by Allergy & Anaphylaxis Australia. Allergy & Anaphylaxis Australia continue to refine their marketing strategy to raise consumer awareness and engagement with the organisation.

Eczema Connect® pilot
The Eczema Connect® program started in December 2024 and is being piloted in Western Australia. The program provides online education and support to help people manage their eczema during the time between referral to a specialist, and their specialist appointment. Allergy & Anaphylaxis Australia will complete the pilot and evaluate the Eczema Connect® program.

Recognition pathways for allergy healthcare professionals
Develop processes to verify healthcare professionals who have additional training and experience in allergy. This will make it easier for people with allergies and their carers to find a healthcare professional who has completed recognised allergy training.

MBS item number for drug challenges
ASCIA will apply to the Government for a Medicare Benefits Schedule (MBS) item number for drug (medication) challenges. There are long waiting times for drug challenges in the public system. With an MBS item number, more people should have access to drug challenges in private allergy specialist clinics.

allergy assist® pilot
allergy assist® is a new education and advice platform which was launched in February 2025. General practitioners and rural generalists can get direct advice from a clinical immunology/allergy specialist on a patient with an allergic condition within 48 hours, helping them to manage patients locally, where possible. The National Allergy Council will complete a 12 month pilot and evaluation of allergy assist®.

Digital education and support programs for consumers
Allergy & Anaphylaxis Australia will continue to promote, deliver and maintain digital education and support programs for allergic rhinitis (hay fever), food allergy and eating out with food allergy. They will develop new programs for insect allergy and post (after) anaphylaxis.

Visibility of verified allergy healthcare professionals
The National Allergy Council is working with Provider Connect Australia and Healthdirect to make healthcare professionals with verified allergy training visible in the National Health Service Finder.

Allergy care closer to home
Engage with decision-makers about how allergy services are delivered to people living in rural, regional and remote areas. Advocate for greater uptake of models of care that have been shown to improve access to allergy services locally.

Allergy Care and Education (ACE) Nurse pilot
Develop and pilot Allergy Care and Education (ACE) Nurse services in regional and rural areas. This initiative will train and support nurses working in doctors’ practices and community health to help people with allergies use their treatments correctly, and collect information on the services they provide.

National standards and guidelines for allergy
Develop a standard that describes what patients and carers can expect when accessing allergy care. Develop a guideline for the recording, transfer and access of allergy information in electronic health records.

Allergy referral resources
Develop a referral toolkit with standardised information for doctors who refer patients to hospital allergy departments and private allergy specialist clinics, to improve referral processes to allergy services.
Stay informed
Subscribe to the Shared Care for Allergy Bulletin.
Follow the National Allergy Council social media on Facebook, Instagram, or LinkedIn.